Meckel's diverticulum causing acute intestinal obstruction: A case report and comprehensive review of the literature
Abstract
Introduction: Meckel’s diverticulum is a congenital anomaly that is often detected incidentally. When it presents symptomatically, it causes painless gastrointestinal bleeding.Nevertheless, in rare instances, it can cause acute intestinal obstruction, often obscuring the true clinical picture.
Case presentation: A 31-year-old male presented to the emergency department with a 24-h history of unremitting nausea, biliary emesis, abdominal distension, and absolute constipation. After ruling out the most common etiologies of acute bowel obstruction, radiological imaging was obtained and was suggestive of meckel’s diverticulum. Laparoscopic meckel’s diverticulectomy was performed, with the subsequent histopathological analysis confirming ectopic gastric tissue.
Discussion: Meckel’s diverticulum occurs consequent to incomplete obliteration of the vitelline or omphalomesenteric duct, which connects the developing intestines to the yolk sac. It is found in roughly 2% of the population, of which only about 4% may become symptomatic due to any number of complications. Specifically, small bowel obstruction (SBO) and diverticulitis secondary to ectopic gastric or pancreatic tissue are the most common presentations of symptomatic MD.
Conclusion: Although relatively rare in adults, MD should be considered in the list of differentials in patients with intussusception leading to SBO, especially on a background history unremarkable for the most common etiologies causing SBO including post-operative adhesions and hernias.
Introduction
Acute intestinal obstruction continues to be a medical and surgical emergency that warrants an emergency intervention. Acute bowel ob- struction usually presents with a vague constellation of symptoms, of- ten characterized by bilious/non-bilious emesis, nausea, vomiting, anorexia, and abdominal pain [1]. While postoperative adhesions and tumors afflicting the bowel remain leading causes of acute intestinal ob- struction, rarer entities, such as Meckel’s diverticulum, can seldom be the source, often obscuring the true clinical picture [2,3]. In gastroen- terology literature, post-operative adhesions and hernias are frequently
cited as being the leading causes of small bowel obstruction. However, rare congenital abnormalities such as meckel’s diverticulum are not routinely thought to be the source of acute small bowel obstruction [2,3]. Meckel’s diverticulum (MD) is defined as a congenital anomaly that ensues in the wake of partial closure and persistence of the vitelline, or the omphalomesenteric, duct during embryogenesis [1,2]. This usually occurs in the fifth week of development and causes a true outpouching of the small intestine, located approximately two feet from the ileocecal valve [2,3]. It is the most common congenital abnormality afflicting the gastrointestinal tract and has been reported in up to 1–3% of patients [2]. MD, a true diverticulum, involves all layers of the small

Fig. 1. An abdominal x-ray divulging multiple air-fluid levels within the colon, thus alluding to an obstructive etiology
intestine and is known to contain ectopic gastric mucosa [1]. It is gener- ally asymptomatic and is usually discovered incidentally during surgi- cal exploration of other diseases or less commonly through diagnostic imaging [1]. However, hemorrhagic, inflammatory, and obstructive complications can arise [1–3]. Additionally, MD can present with pain- less bleeding due to ectopic gastric acid and pepsin production in the di- verticulum (gastric mucosa or pancreatic differentiation in MD mu- cosa), further complicating the clinical picture [3,4]. In patients pre- senting with painless gastrointestinal bleeding of unknown etiology, MD may be suspected [2,3]. Nonetheless, acute intestinal obstruction consequent to the presence of meckel’s diverticulum in the adult popu- lation remains a clinical enigma [3,4]. Herein, we elucidate the case of a 31-year-old male who presented with chief complaints of nausea, bil- iary emesis, and abdominal distension on a background of unremark- able medical and surgical history. Further investigative workup di- vulged the presence of meckel’s diverticulum, with subsequent divertic- ulectomy resulting in prompt abatement of the patient’s symptoms. The overarching objective of the present paper is to prompt clinicians to rec- ognize MD as a potential cause of acute small bowel obstruction. Al- though the patient’s age at presentation can yield imperative diagnostic cues, MD should nevertheless be considered in the list of differentials in patients presenting with acute small bowel obstruction regardless of age.
Case Presentation
A 31-year-old male presented to the emergency department with a 24-h history of unremitting nausea, biliary emesis, abdominal disten- sion, and absolute constipation. Notably, the patient’s last regular bowel movement had been three days prior to the current presentation, with the patient erroneously attributing his altered bowel habits to his recent onset of anorexia of unknown origin. The patient reported no red flag symptoms, affirmatively denying recent fevers, previously altered bowel habits, infectious urinary symptoms, or weight loss. The patient’s prior medical and surgical histories were unimpressive, and he reported no other comorbidities. Pertinently, the patient had had an episode sim- ilar to the current one four years ago; at the time, his condition was managed conservatively and resulted in a prompt resolution of his symptoms within 24 hours of his presentation to the hospital. The pa- tient remained asymptomatic thereafter with no consequent episodes till the current presentation.
Upon clinical examination, the patient appeared profusely unwell, with excruciating, 7/10, vague, non-localized abdominal pain that caused significant distress to the patient. Abdominal examination re- vealed a soft, distended abdomen that was non-tender with no evidence of rigidity, peritonitis, or guarding. Pertinently, bowel sounds were au- dible and were noted to be tinkling in nature, raising the initial suspi- cions for an obstructive etiology underlying the patient’s clinical pre- sentation. The murphy’s sign, along with the psoas, obturator, and rovs- ing’s signs, were all negative and unimpressive, effectively ruling out acute cholecystitis and acute appendicitis as plausible etiologies. The patient’s past surgical history was also unimpressive, further precluding post-operative adhesions as the likely etiology. Upon clinical examina- tion, there was no evidence of hernial protrusions, and the genital ori- fices were unremarkable. Furthermore, clinical examination of the ab- domen did not reveal any rigidity or guarding, and no signs of peritoni- tis were appreciated. The patient’s C-reactive protein was raised to 15; however, his remaining labs were unremarkable for any pertinent de- rangements. In order to better delineate the etiology underlying the pa- tient’s presentation, an abdominal x-ray was obtained and revealed multiple air-fluid levels in the small bowel (Fig. 1).
Based on the patient’s x-ray findings, an obstructive pathology was deemed plausible. However, given that the patient demonstrated an un- remarkable surgical history and did not show signs of a possible gas- trointestinal malignancy, adhesions, and tumor as causes of acute in- testinal obstruction were effectively ruled out. Further radiological in- vestigation through the means of a computed tomography (CT) scan di-

Fig. 2. CT scan of the patient’s abdomen showing a transition point in the terminal ileum (red arrow), with mesenteric band cut-off. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
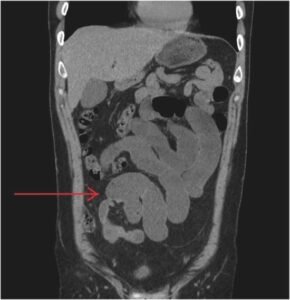
Fig. 3. CT scan of the abdomen showing the presence of meckel’s loops (red ar- row), further alluding to the presence of meckel’s diverticulum. (For interpreta- tion of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
vulged a transition point in the terminal ileum, with mesenteric band cut-off, strongly alluding to the presence of a diverticulum in the speci- fied region (Fig. 2).
The CT imaging of the abdomen further revealed the presence of the classical meckel’s loops, thereby confirming the presence of meckel’s di- verticulum (Fig. 3).
Considering the impression obtained from the patient’s radiological work-up, a multidisciplinary team meeting (MDT) was conducted. The presence of meckel’s diverticulum due to an acute small bowel obstruc- tion was deemed exceedingly plausible. Consequently, the patient was managed using conservative measures for the next 24 hours; however, the patient refused a nasogastric tube, which would have been pivotal in relieving the obstruction. During this time, the patient had an episode of nominal bowel motion once but did not pass any flatus. Conservative treatment was thus continued, and the patient was prepared for a laparoscopic diverticulectomy.
During the operation, meckel’s diverticulum in close proximity to the ileocecal valve was confirmed. Per-operative evaluation divulged meckel’s diverticulitis with the tip attached to the ileal mesentery through the means of a band (Fig. 4).
Given this intraoperative finding, tip and band release was per- formed (Fig. 5).
Additionally, given the presence of meckel’s diverticulitis and the fact that the patient had been symptomatic four years prior to the cur- rent episode, meckel’s diverticulectomy was performed (Fig. 6).
The surgery was conducted unremarkably, with no intra- or periop- erative complications encountered during the process. Postoperatively, the patient remained well and symptom-free except for a minor wound infectious from the hypogastric port used for specimen delivery during the surgery. Daily wound dressings were advised without the need for antibiotics.
The subsequent histopathology report confirmed the presence of dif- fusely inflamed ectopic gastric mucosa in close proximity to the ileoce- cal valve, reinforcing meckel’s diverticulum as the culprit etiology un- derlying the patient’s episode.
The present paper was reported in line with the SCARE guidelines [5].
Discussions
Meckel’s diverticulum (MD) is one of several congenital abnormali- ties that can result from incomplete obliteration of the vitelline or om- phalomesenteric duct, which connects the developing intestines to the yolk sac during development, and is a true diverticulum composed of all intestinal layers [6]. It is found in roughly 2% of the population, of which only about 4% may become symptomatic due to any number of complications [6]. Specifically, small bowel obstruction (SBO) and di- verticulitis secondary to ectopic gastric or pancreatic tissue are the most common presentations of symptomatic MD [7]. When it does pre- sent with obstructive symptoms, subsequent complications may arise in up to 36.5% of cases via a vast myriad of mechanisms [8]. Obstruction can commonly occur due to volvulus or torsion of the intestine around a fibrous band from MD to the umbilicus; intussusception or inversion of the MD into the ileum or cecum; or mesodiverticular band trapping the small bowel under the vascular supply of the MD and potentially lead- ing to strangulation [9]. With symptomatic MD patients representing only 0.08% of the total population, the exceeding rarity of the condition leads to poor rates of pre-operative diagnosis, thereby obscuring the
Fig. 4. Per-operative image delineating meckel’s diverticulitis with the tip attached to the ileal mesentery through the means of a band.
Fig. 5. Intraoperative image demonstrating tip and band release.
Fig. 6. Per-operative image obtained after meckel’s diverticulectomy was performed.
true clinical picture [9]. Early recognition is of paramount importance since a delay in surgery of 36 hours or more can triple the mortality rate from 8% to 25% in patients presenting with strangulation [10]. In this context, it is imperative that clinicians are aware of MD, its associated clinical findings, and the best practices for its diagnosis and manage- ment.
The present study elucidates a case of a 31-year-old male patient with acute onset of symptoms consistent with obstruction. The patient presented with the classical tetrad of bowel obstruction involving nau- sea, emesis, abdominal distension, and constipation [11]. Diagnostic imaging showed multiple air-fluid levels, which indicate pathological accumulation of fluid and gas and are a hallmark finding in X-ray and CT of SBO [12]. Ultrasound for Meckel’s Diverticulum is feasible and can identify mesodiverticular bands as a hyperechoic line, particularly in pediatric patients. However, CT scan was found to be more accurate in determining the cause of small bowel obstruction in adults [13]. In cases with ectopic mucosa in the diverticular outpouch, a Meckel’s ra- dionuclide scan, which injects technetium-99 m as a dye to detect gas- tric tissue, can be performed [14]. A previous study found the transition zone was located near the midline in 80% of patients. In our case, the transition point was identified in the terminal or distal ileum [15].
Interestingly, volvulus of the MD was not suspected as a mechanism of obstruction in our case as there was no fibrous band connecting the
MD to the umbilicus. We also did not suspect intussusception of the small bowel due to the absence of inversion of the diverticular out- pouching into the ileum or cecum. The subsequent histopathology re- port showed unremarkable intestinal tissue. The lack of ectopic tissue thus suggests diverticulitis as a cause of inflammation, and subsequent obstruction was not a likely differential. Instead, the tip of the Meckel’s diverticulum with a band attached to the ileal mesentery was discov- ered per-operatively during the diverticulectomy. Thus, mesodiverticu- lar band (MDB) of Meckel’s diverticulum was determined to be the cause of SBO in this patient. The MDB is a remnant of the vitelline artery, which supplies Meckel’s Diverticulum and provides a bridge for bowel loops to herniate and become strangulated, gangrenous, is- chemic, or otherwise mechanically obstructed [16,17].
Surgery, in specific meckel’s diverticulectomy, remains the mainstay of treatment in such cases. The most common forms are diverticulectomy, wedge, or segmental resection, and the rationale for which procedure to form depends largely on the integrity of the diverticular base and proximal ileum and the location of ectopic tissue if any [3]. Wedge or segmental resection is recommended for MD with SBO; however, diverticulectomy was performed in our patient with full recovery and resolution of symptoms [3]. Generally, prophylactic removal of MD found incidentally is still a controversial topic, with one systematic review of
244 cases divulging reduced postoperative consequences for uncomplicated and asymptomatic Meckel’s Diverticulum left alone [13].
In order to better elucidate the etiology underlying the obstructive symptoms seen in our case, we conducted a literature search using the digital databases (PubMed/MEDLINE, CINAHL, and Web of Science) to search for relevant material and articles implicating MD as a cause of SBO. The literature search in our search was conducted using the terms
(s): “small bowel obstruction” AND “meckel’s diverticulum” OR “diverticulitis” OR “volvulus” OR “intussusception”. The symptomatology, imaging findings, treatment employed, and the follow-up are delineated by Table 1 below [18–59].
Limitations
The present study discusses a case report and delineates a single- center experience dealing with an unusual etiology underlying acute small bowel obstruction. While the study yields important evidence sur- rounding this etiology and prompts the clinicians to aptly recognize this congenital aberration as a cause of acute small bowel obstruction, it is limited by its sample size. Further multi-centric cross-sectional studies evaluating the true, unadjusted incidence of MD as the causative etiol- ogy underlying acute small bowel obstruction will further yield robust data to support the presented conclusions.
Conclusions
MD is the most common congenital abnormality of the gastrointestinal tract, presenting in 1–3% of patients, of which about 4% may become symptomatic. When asymptomatic, it is discovered incidentally during surgical exploration or through diagnostic imaging. Various he- morrhagic, inflammatory, and obstructive complications can arise, leading to an array of presentations. Nevertheless, the presence of MD as the causative etiology underlying acute SBO remains a clinical enigma, with most cases erroneously attributed to post-operative adhe- sions and/or abdominal hernias. Early diagnosis and a high index of suspicion are imperative to deliver the most optimal treatment. Al- though relatively rare in adults, MD should be considered in the list of differentials in patients with intussusception leading to SBO, especially on a background history unremarkable for the most common etiologies causing SBO.




