Endometriotic Stones; Can they exist? A case report
Abstract
Endometriosis is a gynecological pathology that manifests as pelvic pain, infertility and cyclical issues. The presence of endometriotic tissue outside the uterus is the hallmark of endometriosis and commonest sites are ovaries, fallopian tubes, uterosacral ligaments and lateral pelvic peritoneum. Ovarian endometriotic cyst (EC) is typically a chocolate cyst that is often diagnosed by a combination of clinical history, examination and radiological imaging. However, the definitive diagnosis requires histopathological confirmation. The management is complex and requires long term suppression of menstrual cycle and ovarian cystectomy. We hereby illustrate a case of a young female who presented with EC. During a routine daycare laparoscopic cystectomy, a rare finding of endometriotic stones was ascertained per-operatively. Patient remained well post operatively and was discharged in the evening.
Introduction
Endometriosis is a chronic gynecological disease that occurs as a result of endometriotic tissue outside the uterus. 1 Common sites are ovaries, fallopian tubes, uterosacral ligaments and lateral pelvic peritoneum. 2,3 In ovaries, it frequently presents as endometriotic cyst (EC) that is noncancerous and contains chocolate like fluid. 4 EC is often the underlying culprit responsible for chronic pelvic pain associated with ovulation and menstruation in females of reproductive age. 5 The diagnosis of EC requires a combination of good history, clinical examination and investigations such as cancer antigen 125 (CA125) and ultrasound imaging. 1 Although the ultrasonography is generally able to identify EC but definitive diagnosis is based on laparoscopy and histological confirmation. 1,6 Differentials while managing such cysts must include dermoid cyst, hemorrhagic cyst, neoplasms and uncommonly, abscesses and ectopic pregnancy. 7 Management of EC is controversial and depends upon size, symptoms and patient preferences especially when there are concerns for fertility. Long term suppression of menstrual cycle is the mainstay of management for cysts smaller than 3cm while those greater than 3cm are dealt with laparoscopic ovarian cystectomy. 8,9 Patients who have fertility problems are predominantly planned to proceed for ovarian cystectomy. This aids in assisted reproductive methods, alleviates pelvic pain and improves likelihood of successful oocyte retrieval procedure. 10 By virtue of this platform, we hereby report a case of a laparoscopic endometriotic cystectomy which per-operatively revealed endometriotic stones within the cyst cavity, a rare occurrence. It has not been reported previously as per our knowledge.
Case Report
A 30 years old young female, resident of Rawalpindi, presented with cyclical menstrual and pelvic pain in right lower quadrant, dysmenorrhea and irregular cycles for the last two years. Pain aggravated during menstruation and relieved by taking oral non steroidal antiinflammatory drugs. It was not associated with any physical activity, food, anorexia, weight loss, fever, any symptoms related to gastrointestinal or urinary tract. For the past six months, she was under medical management for endometriosis and right ovarian EC. Recently after her wedding, she and her husband had planned for conception. There were no clinical findings except right sided uterosacral ligament tenderness on pelvic examination. CA-125 levels were slightly raised to 58 U/mL. Recent ultrasound showed right adnexal EC of 5.8 x 4.9 x 6.6 cm in size as depicted by Figure 1.

Figure 1: Ultrasound showing right endometriotic cyst (red arrows)
Due to failure of medical management, chronic pain and fertility related concerns; patient was planned for diagnostic laparoscopy and to proceed for laparoscopic cystectomy. Prior to surgery, informed consent was taken for oophorectomy, cystectomy and deroofing of cyst with possibility of recurrence and insufficient ovarian tissue preservation for fertility. Laparoscopy was performed in trendelenburg’s position. Operative findings were consistent with right EC but additionally a rare finding of endometriotic stones was discovered, shown in Figure 2 and Figure 3. Laparoscopic cyst deroofing, followed by cystectomy was performed. Remnant tissue was packed with adrenaline soaked gauze for five minutes. Hemostasis was secured using bipolar electrocautery. Specimen including stones was delivered in bag. Picture of specimens is shown in Figure 4.
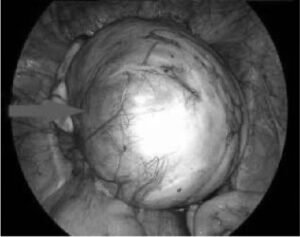
Figure 2: Per-operative image of right endometriotic cyst (red arrow)
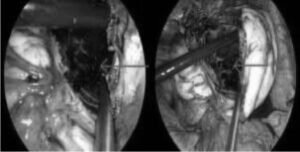
Figure 3: Per-operative image of endometriotic stones (red arrows)

Figure 4: Post operative image showing cyst wall
(blue arrows) and endometriotic stones (red arrows)
Cyst wall was sent for histopathology. Patient was discharged within 24 hours and had unremarkable post-operative recovery.
Histopathology report was consistent with EC.
Discussion
Endometriosis has variable presentations and diagnosis is often delayed. This causes hindrance in proper management and results in vast implications especially on quality of life and daily routine. 11 Laparoscopic ovarian cystectomy is recommended for a symptomatic EC that is without a widespread disease and is greater than 3cm size. Although this provides lowest recurrence rates and highest possibility of spontaneous conception, the risk of insufficient ovarian reserve persists. This is attributed to inadvertent removal of normal ovarian tissue during cystectomy and cauterization to control the bleeding. 9 First choice of imaging in pelvic adnexal pathologies is ultrasonography which is cheap, effective and without any radiation or contrast exposure. CT scan and MRI are superior to ultrasound in assessing the adnexal masses as they help in correlation of surrounding structures and surgical planning. 6 Additionally they are able to differentiate complex cysts, septated lesions, solid masses and benign from malignant pathologies. We did not perform a CT scan or MRI since the clinical diagnosis was quite evident and the size of cyst was not a huge one. Patient was planned for laparoscopic intervention which is considered gold standard for the diagnosis of endometriosis and has the therapeutic advantage of treating endometriotic cysts as well. 12 Our patient had concerns for fertility since she was planning for conception, and endometriosis at any stage is known to decrease fertility. 11 Treatment modalities were discussed with the patient and her husband, and consensus was reached to proceed surgically. Laparoscopically, the cyst is usually aspirated under vision to confirm the diagnosis and to take the sample. Later, suction and irrigation is performed multiple times before proceeding for cystectomy to avoid contamination. In our case, aspiration needle was used to take the sample as well as for suction and irrigation, before carrying out cystectomy. The stones were thus easily seen after deroofing, else they could have easily been missed. Bleeding from the ovarian tissue was packed with adrenaline-soaked gauze, later, hemostatsis was achieved using bipolar cautery. Monopolar or bipolar cautery is an effective method for controlling hemostasis but results in damage to ovarian follicles causing insufficient ovarian reserve.13 Adrenaline-soaked gauze decreases the need for bipolar cautery and its extent, thus improving outcomes related to ovarian reserves. Histopathological confirmation is a requisite for definitive diagnosis and also rules out any underlying malignancy.
Although laparoscopy has the advantage of speedy recovery, minimal scar, diagnostic evaluation of the whole abdominal cavity and staging of the disease, but it has the disadvantage of decreased depth perception of the cyst, loss of tactile feedback, risk of spillage and implantation especially at the port sites.
Laparoscopic technique has the advantage of being diagnostic and therapeutic modality. In addition, it has the capability to stage the disease and identify uncommon findings that can easily be missed otherwise. EC can be managed
laparoscopically if the expertise is available. Care must be taken to avoid port site implantation.
References
- Foti PV, Farina R, Palmucci S, Vizzini IAA, Libertini N, Coronella M, et al. Endometriosis: clinical features, MR imaging findings and pathologic Insights Imaging. 2018; 9:149-172.
https://doi.org/10.1007/s13244-017-0591-0
- Katsoulis IE, Katsoulis IE. Retrorectal endometrioid cyst: a case report. J Med Case Reports. 2010;
4:389-10. https://doi.org/10.1186/1752-1947-4-
389
- Jiao Y, Lu B. Poorly differentiated mucinous carcinoma with signet ring cells in an ovarian endometriotic cyst: a case report. Diagn Pathol.
2019; 14:73. https://doi.org/10.1186/s13000-019-
0850-0
- Hingankar Y, Taksande V and Mahakarkar M. Chocolate Endometrial Cyst: A Case Report. Journal of Pharmaceutical Research International.
2021; 33(40B):1-6.
https://doi.org/10.9734/jpri/2021/v33i40B32254
- Bulun SE, Yilmaz BD, Sison C, Miyazaki K, Bernardi L, Liu S, et al. Endocr Rev. 2019; 40(4):1048-1079. https://doi.org/10.1210/er.2018-00242
- Yaşar L, Sönmez AS, Zebitay AG, Neslihan G, Yazıcıoğlu HF, Mehmetoğlu G. Huge ovarian endometrioma—a case report. Gynecol Surg.
2010; 7:365-367. https://doi.org/10.1007/s10397-
009-0482-6
- Asani L, Nikolova D, Madzunkova K, Karanfilovski V, Pandilov S, Janevska V. Osseous Metaplasia in Ovarian Endometrial Cyst: A case report. 2019; 23(5):17729-17732.
http://dx.doi.org/10.26717/BJSTR.2019.23.003959
- Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat
Rev Endocrinol. 2014; 10:261-275.
https://doi.org/10.1038/nrendo.2013.255
- Akkaranurakkul P, Lertvikool S, Hongsakorn W, Vallibhakara O, Tantanavipas S, Paiwattananupant K, et al. Effects of intravenous tranexamic acid on ovarian reserve and intra–operative blood loss during laparoscopic cystectomy of endometriotic cyst: a pilot randomized controlled trial. Pilot
Feasibility Stud. 2021; 7:171.
https://doi.org/10.1186/s40814-021-00907-y
- Dunselman GAJ, Vermeulen N, Becker C, CalhazJorge C, D’Hooghe T, Bie BD, et al. ESHRE guideline: management of women with Human reproduction. 2014; 29(3):400-412. https://doi.org/10.1093/humrep/det457
- Frankel LR. A 10–Year Journey to Diagnosis With Endometriosis: An Autobiographical Case Report.
Cureus. 2022; 14(1):21329.
https://doi.org/10.7759/cureus.21329
- Young H, Bui T, Cramer SE, O’Connell R, Houshyar R. Ruptured endometrioma in a nonpregnant patient: a case report. J Med Case Reports. 2022; 16:161. https://doi.org/10.1186/s13256-022-03361-3
- Sugita A, Iwase A, Goto M, Nakahara T, Nakamura T, Kondo M, et al. One–year follow–up of serum antimüllerian hormone levels in patients with cystectomy: are different sequential changes due to different mechanisms causing damage to the ovarian reserve?. Fertil Steril. 2013; 100(2):51622. https://doi.org/10.1016/j.fertnstert.2013.03.032



