Recurrent appendicitis of vermiform appendix after a prior appendectomy: A case report and review of the literature
Abstract
Introduction: Acute appendicitis is one of the leading causes of acute abdominal pain and surgical emergency. Stump appendicitis is a known complication of appendectomy whereby a retained appendiceal tip serves as a nidus for recurrent bouts of inflammation. Nevertheless, full-blown appendicitis of the vermiform appendix after a prior appendectomy remains a diagnostic conundrum.
Case presentation: A 45-year-old woman presented with a six-month history of right iliac fossa pain. Pertinently, she had undergone a prior open appendectomy twelve years ago. Further investigative workup revealed full-blown appendicitis, which was not attributable to a retained appendiceal stump. A subsequent laparoscopic appendectomy was performed, and the resultant specimen was sent for further evaluation, confirming the diagnosis of recurrent appendicitis.
Clinical discussion: Acute appendicitis is one of the most common life-threatening abdominal surgical emergencies worldwide, with 300000 appendectomies per- formed annually in the United States alone. Stump and chronic appendicitis are two separate and exceedingly rare clinical entities that may present simultaneously and develop serious complications unless promptly recognized and appropriately managed. The present paper prompts the clinicians to distinguish amongst the two at the initial surgery in order to thwart further exacerbations.
Conclusion: While stump appendicitis is a rare but well-characterized complication of a prior appendectomy, full-blown appendicitis of vermiform appendix remains elusive. It is therefore imperative to distinguish between a duplicated and a recurrent appendix at the initial operative procedure to facilitate optimal patient management.
Introduction
Acute appendicitis remains a leading cause of acute right iliac fossa pain, often presenting as a life-threatening surgical emergency war- ranting prompt surgical treatment. In the United States alone, 300000 appendectomies are performed annually, with the rates soaring even higher in other regions globally [1,2]. Acute appendicitis is thought to result from a myriad of etiologies including obstruction of the appendiceal lumen, bacterial colonization, growth, inflammation, bowel ischemia, or bowel perforation [3]. The definitive pathophysiology is poorly understood and poses a challenge in diagnosing acute appendicitis pre-operatively. The current diagnostic algorithm of acute
appendicitis has been based on initial clinical judgement, followed by imaging and laboratory tests. Acute abdomen symptoms such as right lower quadrant (RLQ) pain, rigidity, and periumbilical pain radiation to the right iliac fossa (RIF) are classic for acute appendicitis [4,5]. In current practice, clinical scoring scales are utilised with supporting laboratory tests and are widely advocated to stratify the risk of acute appendicitis. The most widely accepted scaling systems that guide the management of acute appendicitis consist of the Alvarado score, Pediatric appendicitis Score, or the Appendicitis Inflammatory Response
score [6–10]. The integration of point-of-care ultrasonography has improved the diagnostic accuracy of acute appendicitis and complements the scoring systems [11]. Depending on their disease severity, patients will be managed medically or surgically and can undergo definitive treatment through either open or laparoscopic appendectomy. Though a standard treatment for appendicitis, more commonly reported complications include wound infection, abscess, perforation, and sepsis [12,13]. These risks equate to longer hospital stays and extended hospital stays which can hinder the recovery of patients. However, an underreported and serious complication of appendectomies includes recurrent or chronic appendicitis, which is often misdiagnosed in patients surgically treated for acute appendicitis in the past.
Stump appendicitis, although uncommon, is a relevant and devastating complication of both open and laparoscopic appendectomies. The residual appendiceal tissue after the procedure can become repeatedly inflamed and leaves a stump, predisposing patients to recurrent appendicitis. Although there is no reported incidence, it is presumably thought to be between 0.002% and 0.15% occurring anytime between 5 weeks and 17.5 years postoperatively [4,5]. Despite the low incidence, this still represents a commonly overlooked cause of RIF pain in patients with prior appendectomies and is usually not considered a preliminary diagnosis [6]. An appendiceal stump poses a dilemma to clinicians and is commonly associated with a late diagnosis if one is unaware of the uncommon clinical presentations that distinguish a stump from acute appendicitis [7]. Despite newer imaging modalities and technology, pre-operative diagnosis of appendiceal stumps remains a clinical conundrum and is associated with an increased risk of perforation due to a delay in referral and management [8]. The etiology of stump appendicitis is unclear but thought to be predisposed by medical and surgical factors following a previous appendectomy. However, another diagnostic dilemma leading to recurrent appendicitis is the possibility of an underlying duplicated appendix, which may be overlooked during initial preoperative and peri-operative workup. This congenital anomaly was first reported in 1892 and since then, has been reported as an incidental finding that was commonly “missed” in pre-operative investigations [9,10]. The reported incidence rate of the duplicated appendix is exceedingly low, hovering around 0.004% [7]. However, thorough exploration of the caecum during laparotomy can avoid delayed diagnosis, serious complications, and medicolegal consequences in the future [8].
Herein, we chronicle the case of a 45-year-old female patient presenting with a constellation of symptoms typical of acute appendicitis on a background history of prior appendectomy. Second laparoscopic appendectomy confirmed a single appendectomy scar in the colon, reaffirming the diagnosis of a regrown, rather than a duplicated, vermiform appendix. The present paper was reported in accordance with the SCARE guidelines [9].
Case Presentation
A 45-year-old woman presented to the hospital with a six month history of intermittent right iliac fossa (RIF) pain. The patient denied experiencing nausea, vomiting, urinary or bowel symptoms and had undergone open appendectomy twelve years prior to the current pre- sentation. Pertinently, investigative workup at the time had excluded the possibility of appendiceal duplication, and subsequent open ap- pendectomy further reaffirmed this notion. Upon physical examination, the patient demonstrated mild tenderness in the RIF with positive rebound tenderness. The rovsing’s sign was negative at the time, with no evidence of rigidity, guarding, or peritonitis. The patient also had a well healed grid-iron scar in the RIF from her previous open appendectomy. Ultrasound imaging of the RIF showed a complex ovarian mass and further non-contrast computed tomography (CT) scans (Fig. 1 and Fig. 2) revealed enhancement and thickening at the splenic flexure as well as a tubular, blind-ended structure in the RIF resembling an ap- pendix which was noted to be dilated, fluid-filled with a caliber of 10 mm. The structure showed thickened walls with surrounding mild free fluid present. Given the presence of a complex ovarian mass, CA-125 levels were obtained and were borderline raised. However, a
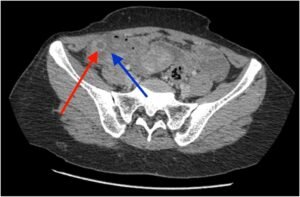
Fig. 1. Axial view.

Fig. 2. A coronal non-contrast CT scan.
subsequent colonoscopy and barium follow-through yielded normal results and effectively excluded the presence of an ovarian malignancy. Non-contrast abdominal CT demonstrating an inflamed appendix (red arrow) and peri appendiceal collection and stranding (blue arrow).
The inflamed appendix can be seen (yellow arrow), with peri appendiceal stranding and fibrosis. Non-contrast CT scanning of the abdomen and the RIF divulged dilated thick walled, fluid-filled tubular structure in the RIF with mild free fluid and lymphadenopathy with the largest lymph node measuring 14 × 9.2 mm in size, likely indicative of acute/subacute appendicitis. Another possible differential for the imaging finding is a simple left adnexal cyst, which was also evaluated (Fig. 3).
Thereafter, the patient was admitted and prepared for a diagnostic laparoscopy and laparoscopic appendectomy. Per-operatively, an acute inflamed appendix filled with pus was seen adherent to the lateral wall near the iliac vessels (Figs. 1–3). Fig. 4 further demonstrates the presence of diffuse adhesions.
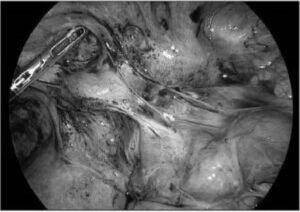
Fig. 3. Inflamed appendix can be visualized along with surrounding adhesions.
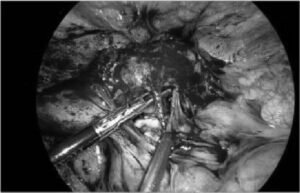
Fig. 4. Further evidence of adhesions, indicative of chronic infections, can be seen per-operatively.
Interestingly, laparoscopy divulged evidence of blunt dissection at the appendiceal tip (Fig. 5).
The tip of the appendix was adherent to the round ligament and 20 mL of reactionary fluid was found in the Pouch of Douglas. A simple left ovarian cyst measuring 3 × 2 cm was also incidentally found. The fal- lopian tubes, ovaries and uterus were unremarkable, and per-operative findings pragmatically precluded the presence of a concomitant malig- nant process. Intraoperatively, the appendix was resected after ligating the bade (Fig. 6).
Finally, a drain was placed at the stump site (Fig. 7).
The patient was discharged in the evening and postoperatively she recovered well with no postoperative complications. Histopathological analysis of the appendix showed extensive fibrosis, and moderate acute and chronic inflammation with serositis, strongly indicating a full-blown inflammatory process involving the appendix. There was no evidence of
malignancy or parasitic infection. The patient continues to do well to date, with no further exacerbations.
Discussion
We highlight a unique case presenting with 6-month history of intermittent appendiceal colic occurring 12 years post-open appendec- tomy. To further clinical understanding of atypical appendicitis, this discussion will address the different forms discovered in our review of the literature and attempt to delineate some of the uncertainty around this topic. While acute appendicitis is well-recognized and a top differ- ential for right lower quadrant pain there is far less known regarding atypical presentations of appendicitis such as chronic and recurrent stump appendicitis and indeed, little concordance in the literature regarding their definitions [10].
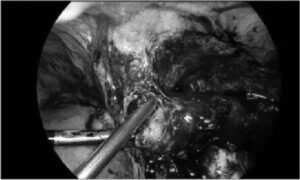
Fig. 5. Blunt dissection at the appendiceal tip.
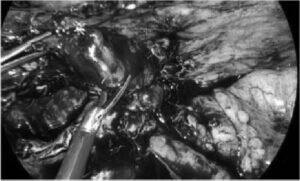
Fig. 6. Resecting the appendix after ligation at the appendiceal base.
Stump and chronic appendicitis are two separate and exceedingly rare clinical entities that may present simultaneously, as in our case, and develop serious complications unless promptly recognized and appro- priately managed. In the literature, both are sometimes referred to as recurrent appendicitis [11,12] however in this paper we refer to stump and recurrent appendicitis interchangeably. Stump appendicitis occurs due to inflammation of the residual appendiceal stump occurring any- where from several days to years after the initial appendectomy [13]. The disease course of stump appendicitis can mirror chronic appendiceal inflammation, as both present with recurrent symptoms requiring additional investigations. Moreover, similar clinical presentations of stump appendicitis to primary acute appendicitis can create difficulty in its diagnosis and prolong immediate treatment.
There is yet another possible differential of recurrent appendicitis occurring in a duplicated appendix after prior appendectomy [14]. Duplicated appendices occur with an estimated incidence of 0.004% and to date, there are 4 main types of appendiceal duplications known ac- cording to Cave–Wallbridge classifications; Type A, B, C and D. Most
pertinent to our case, Type B duplications involving duplicated appendices on either side of the ileocecal valve (B1) or a normally located
appendix followed by a second retrocecal appendix (B2) were distinct diagnostic possibilities [14]. However, the initial resection was con- ducted upon open appendectomy and there was only a singular incision site left on repeat surgery. As such, the possibility of appendiceal duplication was ruled out from our case and we maintain that this was indeed a rare case of stump appendicitis.
The treatment for appendicitis remains appendectomy performed either open or laparoscopically. Despite the reduced visual field, lapa- roscopic appendectomies have several benefits including lower rates of complications, faster postoperative recovery [15] and a previous liter- ature review found only 34% of recurrent stump appendicitis cases were followed by initial laparoscopic appendectomy [4].
Atypical appendicitis, especially following previous appendectomy, is often misdiagnosed and conservative treatment with antibiotics can delay, mask or transiently resolve symptoms only for patients to return on repeat onset of RIF pain [3]. Previous studies have shown it is often misdiagnosed as constipation and gastroenteritis [16] and delayed diagnosis has been associated with perforations, small bowel obstruc- tion, abdominal abscesses and even adenocarcinoma of the residual stump [17].
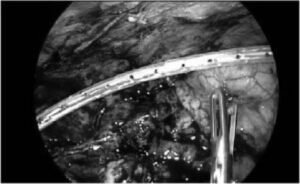
Fig. 7. Intraoperative laparoscopy image demonstrating drain placement at the stump site.
In order to better elucidate the aetiology underlying the recurrent appendicitis observed in the present case, we conducted a literature search using the digital databases (PubMed/MEDLINE, CINAHL, and Web of Science) to search for relevant material and articles reporting any cases and advancements in the diagnosis and management of recurrent full-blown appendicitis. The literature search was conducted using the terms(s): “recurrent appendicitis” AND “vermiform appendix”
OR “stump appendicitis” OR “appendiceal duplication”. The symptomatology, imaging findings, treatment employed, and the follow-up are delineated by Table 1 below [19–69].
While most studies in our review were able to identify stump
appendicitis using CT imaging (Table 1), some resorted to diagnostic laparotomies. In one case where conservative management was repeatedly pursued, the patient experienced 3 episodes of undiagnosed chronic recurrent stump appendicitis until eventual diagnostic laparotomy and subsequent appendiceal stump resection resolved all symptoms [18]. As such, we recommend clinicians consider atypical appendicitis in any patient presenting with RLQ pain regardless of prior appendectomy and withhold antibiotics in favour of full workup including radiological investigation followed by laparoscopic exploration if needed. In addition, we reiterate prior recommendations emphasizing the importance of correct identification of the appendiceal base and ensuring post-resection stump length of no more than 3 mm for any resected appendices ≤6.5cm in length to avoid future stump appendicitis [13].
Limitations
The overarching limitation in our cases was, upon index surgery, the presence of a duplicated appendix was not precluded. As such, it could be the case that the recurrent appendicitis could be afflicting the duplicated, rather than a regrown, appendix. In order to curb this possibility, surgeons should be cognizant of this anatomical aberration and should therefore exclude appendiceal duplication at the time of the index surgery.
Conclusion
While stump appendicitis is a rare but well-characterised complication of a prior appendectomy, full-blown appendicitis of vermiform appendix remains elusive. It is therefore imperative to distinguish be- tween a duplicated and a recurrent appendix at the initial index operative procedure to facilitate optimal patient management. Correctly identifying the appendiceal base during surgery and ensuring a post- resection stump length of no more than 3 mm can preclude the possibility of stump appendicitis. Furthermore, surgical incision sites should be evaluated during repeated appendectomies to distinguish an appendiceal duplication from stump appendicitis to better dictate optimal patient management.



